Acute Mesenteric Ischemia
Thrombolysis
What is thrombolysis?
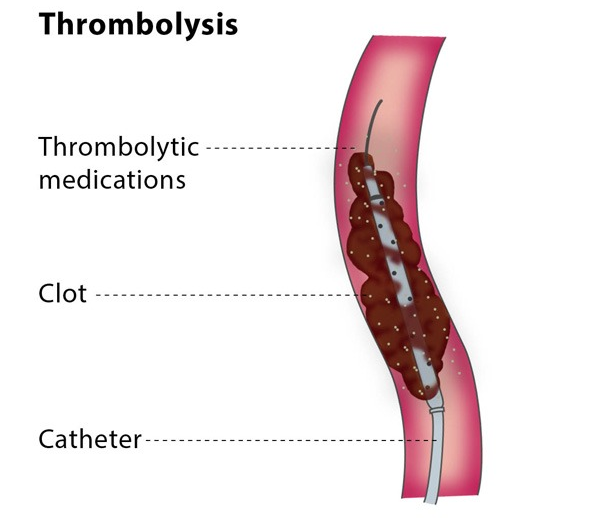
Thrombolysis is a procedure which uses medication to dissolve a blood clot. The medications used in thrombolysis are called thrombolytic agents.
Thrombolysis is most commonly performed to treat a blood clot in the lower limbs, which causes acute limb ischaemia (restricted blood flow in the affected limb), leading to pain in affected area. It can also be used to treat blood clots in organs such as the liver or kidney, as well as treating restricted blood flow in the small intestine due to inflammation or an injury, massive pulmonary embolism (a blood clot in main artery of a lung) or stroke.
How does the procedure work?
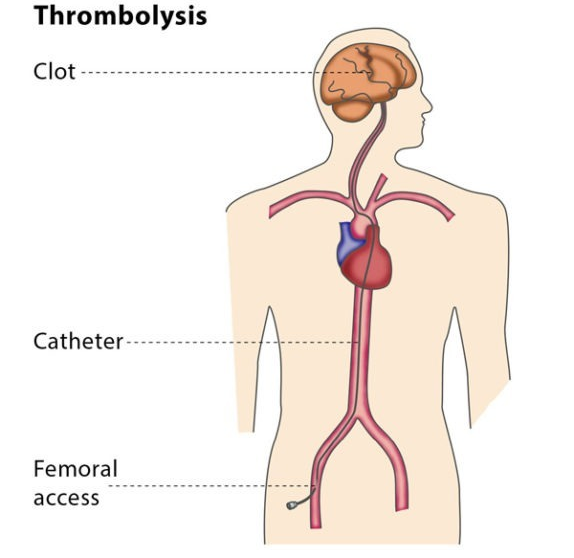
The interventional radiologist will insert a 3 mm plastic tube (called a sheath) into the base of your skull or your groin and will guide the sheath to the blood clot.
Thrombolysis is performed using medications which prevent blood clots from growing (known as lytic substances), which are administered via a catheter into the thrombus. Catheters designed to be used in this treatment have lots of tiny holes. This means that the distribution of lytic substances can be spread out across the catheter and have maximum effect.
Why perform it?
What are the risks?
Bibliography
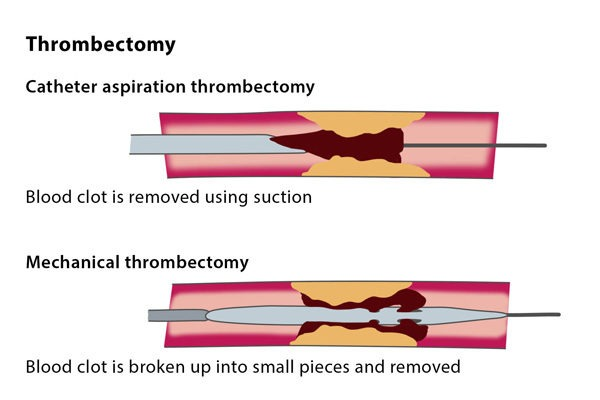
Thrombectomy
What is an endovascular thrombectomy?
How does the procedure work?
Why perform it?
What are the risks?
Bibliography
- Ansel GM, George BS, Botti CF, McNamara TO, Jenkins JS, Ramee SR, et al. Rheolytic thrombectomy in the management of limb ischemia: 30-day results from a multicenter registry. Journal of endovascular therapy: an official journal of the International Society of Endovascular Specialists. 2002; 9(4):395-402.
2. Allie DE, Hebert CJ, Lirtzman MD, Wyatt CH, Keller VA, Khan MH, et al. Novel simultaneous combination chemical thrombolysis/rheolytic thrombectomy therapy for acute critical limb ischemia: the power-pulse spray technique. Catheterization and cardiovascular interventions: official journal of the Society for Cardiac Angiography & Interventions. 2004; 63(4):512-22.
3. Kasirajan K, Gray B, Beavers FP, Clair DG, Greenberg R, Mascha E, et al. Rheolytic thrombectomy in the management of acute and subacute limb-threatening ischemia. Journal of vascular and interventional radiology: JVIR. 2001; 12(4):413-21.
4. Kasirajan K, Haskal ZJ, Ouriel K. The use of mechanical thrombectomy devices in the management of acute peripheral arterial occlusive disease. Journal of vascular and interventional radiology: JVIR. 2001; 12(4):405-11.
5. Wagner HJ, Muller-Hulsbeck S, Pitton MB, Weiss W, Wess M. Rapid thrombectomy with a hydrodynamic catheter: results from a prospective, multicenter trial. Radiology. 1997; 2 05(3):675-81.