Percutaneous Radiographic Gastrostomy (PRG / PEG)
Infinity Intervention Clinic > Departments > Gastroenterology (Digestive System) > Percutaneous Radiographic Gastrostomy (PRG / PEG)
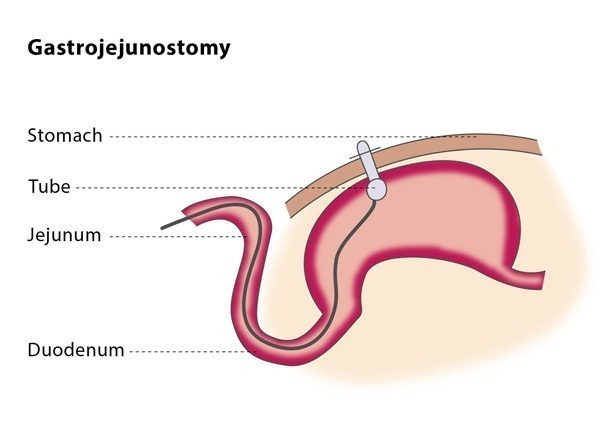
Gastrojejunostomy
What is a gastrojejunostomy?
A gastrojejunostomy is a minimally invasive procedure in which a long catheter-like tube (called a gastrojejunostomy tube) is inserted through your abdomen and into your small intestine. The tube provides nutritional support to patients who are unable to eat and are unsuitable for a gastrostomy tube due to a blockage preventing food from passing from the stomach into the small intestine, severe paralysis of part of the stomach or a high risk of choking.
How does the procedure work?
If you are on any medication which prevents blood clotting, you will stop taking it before the procedure, if possible.
You should not eat anything before the procedure. The interventional radiologist will insert a tube in your nose which will go into your stomach (called a nasogastric tube) and then will perform an ultrasound of your stomach to check the position of your liver and confirm that the tube is correctly placed
The procedure is usually performed under local anaesthesia or moderate sedation. You may be given antibiotics to prevent infection, but this is not always necessary. You will lie on your stomach on a C-arm table, a table designed to be used in imaging procedures.
The procedure is similar to that of percutaneous gastrostomy. In most cases, you will be given an injection of glucagon hydrochloride, which temporarily paralyses the muscles in your stomach. The stomach puncture in gastrojejunostomy is aimed at the area where your stomach connects with your small intestine as this is where the tube will go.
The interventional radiologist will then insert a catheter along with a guidewire into the jejunum, which is the middle section of your small intestine. The guidewire will then be exchanged for a stiffer guidewire. The interventional radiologist will insert some dilators which will expand the area, creating enough space for the gastrojejunostomy tube, which is positioned over the stiff guidewire. The interventional radiologist will inject a few milliliters of contrast media through the gastrojejunostomy tube so that the position of the tube can be confirmed using fluoroscopy.
You will probably be required to stay in hospital overnight, although a gastrojejunostomy can also be performed as an out-patient procedure. You may experience slight discomfort at the entry point of the catheter for the first few hours following the procedure. The location of the tube will be checked daily for signs of leakage or infection. You will be allowed to eat between 8-24 hours after the gastrojejunostomy, after you have consumed 50 ml of water per hour for at least four hours without any negative effects. The T-fasteners used in the procedure can be safely removed 10-14 days after the procedure.
Why perform it?
The indications that a gastrojejunostomy may be beneficial for you are similar to those for a gastrostomy – you may be advised to have this procedure if you are unable to eat normally. The most common reasons for this are neurological causes (such as stroke or dementia), anatomical situations (such as during correction procedures of cleft lip and palate anomalies) and if a blockage is preventing food passing from your stomach to your small intestine.
Because gastrojejunostomy is associated with a reduced risk of aspiration pneumonia, your doctor may recommend it instead of a gastrostomy if you suffer from chronic acid reflux. If the interventional radiologist cannot access your stomach for the gastrostomy tube placement or you have previously had a gastrectomy (the surgical removal of all or part of your stomach), they may directly puncture your jejunum (the middle part of your small intestine) instead – this is known as a jejunostomy.
The reasons why this procedure may not be suitable for you are also similar to those for a gastrostomy. You should not undergo the procedure if you have a blood-clotting disorder, if your colon or liver is positioned between your stomach and abdominal wall (as this prevents a safe access route), if you have peritonitis (inflammation of the thin tissue wall which covers most of your abdominal organs as well as the inner abdominal wall), or if you suffer from untreatable massive ascites (abnormal fluid in your abdomen).
This procedure may not be suitable for you if you have dilated blood vessels in your gullet or stomach, changes in the top layer of the stomach lining, if you have abnormal cell growth in the wall of your stomach, cancer that affects the lining of the abdominal cavity, if you are morbidly obese or if you have had previously had surgery in the area.The technical success rate ranges from 85-95%.
What are the risks?
The possible complications for a gastrojejunostomy are similar to those for a gastrostomy procedure: peritonitis (inflammation of the thin tissue wall within your abdomen), skin infection around the catheter entry site and bruising. As long as you are suitable for the procedure and the interventional radiologist chooses the technique most suited for you, the risk of complications is low (the rate of procedure-related mortality is 2.4%).
Bibliography
- Given MF, Hanson JJ, Lee MJ. Interventional radiology techniques for provision of enteral feeding. Cardiovasc Intervent Radiol 2005; 28(6):692-703.
2. van Overhagen H, Schipper J. Percutaneous jejunostomy. Semin Intervent Radiol 2004; 21(3): 201-206.
3. Bell SD, Carmody EA, Yeung EY, et al: Percutaneous gastrostomy and gastrojejunostomy: additional experience in 519 procedures. Radiology 1995; 194:817-820.
4. Hallisy MJ, Pollard JC. Direct percutaneous jejunostomy. J Vasc Intervent Radiol 1994; 5:625-632.