Trans Arterial Chemo Embolization (TACE) (HCC, NET)
Embolization Therapy for Liver Cancer
Embolization is a procedure that injects substances directly into an artery in the liver to block or reduce the blood flow to a tumor in the liver.
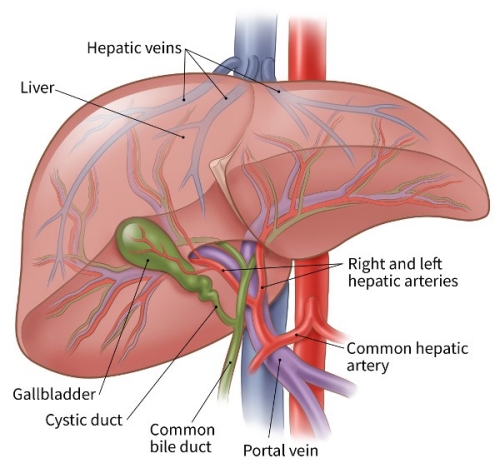
The liver is special in that it has 2 blood supplies. Most normal liver cells are fed by the portal vein, whereas a cancer in the liver is mainly fed by the hepatic artery. Blocking the part of the hepatic artery that feeds the tumor helps kill off the cancer cells, but it leaves most of the healthy liver cells unharmed because they get their blood supply from the portal vein.
Embolization is an option for some patients with tumors that cannot be removed by surgery. It can be used for people with tumors that are too large to be treated with ablation (usually larger than 5 cm across) and who also have adequate liver function. It can also be used with ablation. Embolization can reduce some of the blood supply to the normal liver tissue, so it may not be a good option for some patients whose liver has been damaged by diseases such as hepatitis or cirrhosis. It isn’t yet clear which type of embolization has a better long-term outcome.
People getting this type of treatment typically do not stay in the hospital overnight.
Trans-arterial embolization (TAE)
During trans-arterial embolization a catheter (a thin, flexible tube) is put into an artery in the inner thigh through a small cut and eased up into the hepatic artery in the liver. A dye is usually injected into the bloodstream to help the doctor watch the path of the catheter. Once the catheter is in place, small particles are injected into the artery to plug it up, blocking oxygen and key nutrients from the tumor.
Trans-arterial chemoembolization (TACE)
Trans-arterial chemoembolization is usually the first type of embolization used for large liver cancers that cannot be treated with surgery or ablation. It combines embolization with chemotherapy (chemo). Most often, this is done by giving chemotherapy through the catheter directly into the artery, then plugging up the artery, so the chemo can stay close to the tumor.
Drug-eluting bead chemoembolization (DEB-TACE)
Drug-eluting bead chemoembolization combines TACE embolization with drug-eluting beads (tiny beads that contain a chemotherapy drug). The procedure is essentially the same as TACE except that the artery is blocked after drug-eluting beads are injected. Because the chemo is physically close to the cancer and because the drug-eluting beads slowly release the chemo, the cancer cells are more likely to be damaged and die. The most common chemo drugs used for TACE or DEB-TACE are mitomycin C, cisplatin, and doxorubicin.
Trans-arterial chemoembolization (TACE)
Embolization is a treatment that blocks or slows down the blood going to tissues or an organ. It can be used to block the flow of blood to a tumour so the cancer cells die. When the material used to block the blood supply also delivers chemotherapy drugs to the tumour, it is called chemoembolization. Transarterial chemoembolization (TACE) is a specific type of chemoembolization that blocks the hepatic artery to treat liver cancer.
Liver cancer tumours can grow new blood vessels (called angiogenesis). These blood vessels get most of their blood supply from the hepatic artery, while the rest of the liver tissue gets blood from the portal vein. Because of this, doctors can block the hepatic artery to cut off the blood supply to the tumour without affecting the rest of the liver as long as blood is normally flowing toward the liver in the portal vein.
You will be offered TACE only if you have good liver function, you don’t have any fluid in your abdomen (called ascites) and there are no blood clots in the portal vein (called portal vein thrombosis). TACE may be used if the liver cancer can’t be removed with surgery, can’t be treated with ablation therapy and hasn’t spread to the major blood vessels in the liver or other parts of the body. You may also be offered TACE to keep a liver tumour small if you are waiting for a liver transplant (called bridging therapy).
Doctors may offer TACE to treat liver tumours that are larger than 5 cm, but it may take many treatments to shrink these larger tumours. If cancer is in both lobes of the liver, doctors will treat one lobe at a time. Treatment to each lobe is usually given a month apart so that you have time to recover from the previous TACE treatment.
How TACE is done
TACE is done in the x-ray department of a hospital. You may be given a local anesthetic and medicines to help you relax, or you may be given a general anesthetic to put you to sleep.
The doctor places a thin, flexible tube (called a catheter) into an artery in the groin (called the femoral artery). The doctor then moves the catheter up through the artery until it reaches the hepatic artery in the liver. A dye is injected into the catheter and an x-ray (called an angiogram) is taken to find the branches of the artery that are feeding the liver tumour. The doctor then moves the catheter to these arteries. The doctor injects a material into the arteries feeding the tumour to block them.
The most commonly used material for TACE is a gelatin sponge. Sometimes the gelatin sponge is soaked in a chemotherapy drug before the doctor injects it into the artery. The drug is given directly to the tumour while the gelatin sponge blocks the blood supply to the tumour.
DEB-TACE is a new way of delivering chemotherapy during TACE. It uses special beads that are filled with a chemotherapy drug (called drug-eluting beads, or DEBs). After these beads are injected into the arteries in the liver, they slowly release the drug to treat the tumour. DEBs are as effective as using the sponge or injecting chemotherapy drugs in the arteries. DEB-TACE may have fewer side effects than the other methods.
Chemotherapy drugs used in TACE
There are no standard recommended chemotherapy drugs for TACE. The drugs that may be used alone or together are:
- doxorubicin
- cisplatin
Side effects
Side effects can happen with any type of treatment for liver cancer, but everyone’s experience is different. Some people have many side effects. Other people have only a few side effects.
TACE may cause side effects because it can damage healthy cells as it kills cancer cells. Side effects can develop any time during, immediately after or a few days or weeks after chemotherapy. Most side effects go away on their own or can be treated, but some side effects may last a long time or become permanent.
Side effects will depend mainly on the number of tumours being treated, the amount of scarring in the liver (called cirrhosis) and your overall health.
TACE for liver cancer may cause post-embolization syndrome, which is a group of symptoms that includes:
- fever
- painin the upper-right abdomen, under the ribs
- nausea and vomiting
- fatigue
TACE can also cause:
- bruising or bleeding at the catheter site
- hair loss
- lowered ability to fight off infections
- abnormal liver function
- inflammation of the gallbladder or bile ducts
- a collection of pus in the place where the tumour was destroyed (called an abscess)
- liver failure, especially in advanced cirrhosis
Tell your healthcare team if you have these side effects or others you think might be from TACE. The sooner you tell them of any problems, the sooner they can suggest ways to help you deal with them.
Radioembolization (RE)
Radioembolization combines embolization with radiation therapy. This is done by injecting small beads (called microspheres) that have a radioactive isotope (yttrium-90 or Y-90) attached to them into the hepatic artery. Once infused, the beads lodge in the blood vessels near the tumor, where they give off small amounts of radiation to the tumor site for several days. The radiation travels a very short distance, so its effects are limited mainly to the tumor.
Possible side effects of embolization
Possible complications after embolization include:
- Abdominal pain
- Fever
- Nausea
- Infection in the liver
- Blood clots in the main blood vessels of the liver
Sometimes, it can take 4-6 weeks to fully recover from the procedure. Because healthy liver tissue can be affected, there is a risk that liver function will get worse after embolization. This risk is higher if a large branch of the hepatic artery is embolized. Serious complications are not common, but they are possible.
Disclaimer: All rights reserved to the owner of the content. We are using it just for educational purpose.